Take Preventative Measures This Breast Cancer Awareness Month
A strong family history of breast cancer made one writer get serious about preventive measures.
The “big C” runs in my family. Both my parents passed away at 60 from the disease (my mother from breast cancer and my father from a lung sarcoma), and my only aunt is a breast cancer survivor. While my mom and aunt hadn’t been tested for BRCA1 or BRCA2 gene mutations—which are responsible for about 25 per cent of all hereditary cancers—and I don’t carry the mutation, it’s fair to say that I’m at a genetically elevated risk.
Being a health writer has turned me into a bit of a hypochondriac regarding all ailments, and breast cancer has always topped my list of concerns. However, it took losing a 34-year-old friend last year to Stage 4 breast cancer to bring to light how the disease can strike at any age. At 43, I decided it was time to start being more proactive about my health instead of just worrying about getting a diagnosis.
To do this, I combined my personal research with advice from my medical doctors. My first stop was to revisit thermography, which I tried four years ago on the advice of my OB/GYN, who said that, given my history, it was a safe additional screening procedure to complement my biannual mammograms and ultrasounds. I was worried about relying on mammograms alone, as they don’t always catch breast cancer early enough and sometimes, as was the case with my mother and friend, even miss it completely.
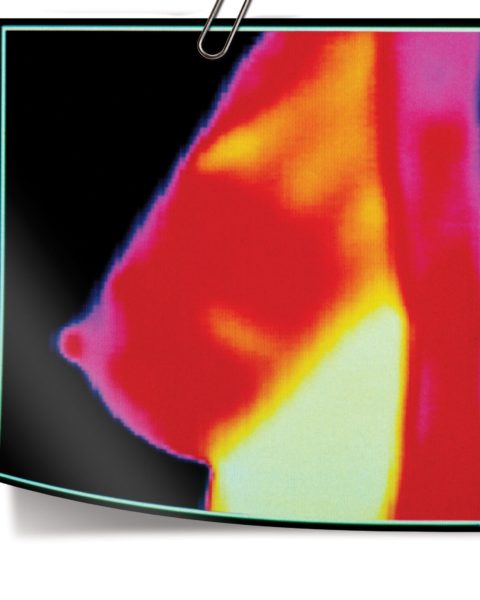
Very dense breast tissue can make it hard to see tumours. Thermography uses a digital infrared scanner to look for heat or inflammation near the surface of the skin, as it’s thought that fast-growing cells, such as cancer cells, create more heat than normal cells. Excess heat will give your breasts a ranking between TH1 (lowest risk) and TH5 (highest risk) and could help you assess your breast cancer risk.
Doctors also look for symmetry between the breasts. Even at a TH2 level, if the heat mapping between the breasts is unilateral, it warrants a visit to your doctor, where you can ask for a breast exam, mammogram and/or ultrasound—regardless of your age. Now, inflammation doesn’t necessarily mean cancer; it simply means an increase in probability. Another limitation of the test is that it costs about $250 per session, whereas mammograms and ultrasounds are covered by government insurance.
A 2008 study published in The American Journal of Surgery found that high-resolution digital infrared imaging is a safe and practical addition to clinical breast exams and mammography, especially for women with dense breast tissue. Dr. Alexander Mostovoy, author of Breast Cancer Is a Preventable Disease, also sees thermography as a valuable tool. “If your thermography report comes back saying you are at an elevated risk, speak with a health care provider to lower your risk while preventive measures are still highly effective,” he says.
Preventive measures could include eating properly and exercising to improve your immune function. Research shows that between 30 and 40 per cent of cancers can be linked to diet, which has an impact on us not only through the chemicals and macronutrients we consume, but also by causing obesity, which is another cancer risk factor. And, according to a 2014 article in Nutrition Journal, the overconsumption of refined sugars, artificial sweeteners, salt, saturated fats, gluten and genetically modified foods impairs the body’s immune system and increases inflammation, both of which increase the risk for the disease.
In addition to eating well and exercising to reduce one’s cancer risk, there’s another often overlooked factor: emotional, physical and environmental stress. “In this day and age, many of us have some degree of cortisol dysregulation,” says Kristy Prouse, MD, FRCS(C), OB/GYN and chief medical officer at the Institute for Hormonal Health in Oakville, Ont. This means that cortisol—our stress hormone—levels can be elevated at the wrong times of the day and too low at others, which can compromise immunity and impact many other hormones.
“Estrogen dominance is one of the risk factors for breast cancer,” says Prouse. After my uneven thermography results (both breasts were TH2, but the pattern of inflammation was different), I decided to get my hormones tested. It came back that I was estrogen-dominant and my progesterone was extremely low. When it comes to hormones, progesterone is the “mother hormone” at the top of the chain. “When progesterone is depleted, hormones downstream from it may also deplete,” says Prouse, adding that symptoms of estrogen dominance include heavy periods, breast tenderness, PMS, fibroids and endometriosis, among others.
I decided to look into bioidentical hormone therapy on the recommendation of my OB/GYN to help balance out my estrogen-to-progesterone ratio. Unlike synthetic hormones, bioidentical hormones have the same molecular structure as those found in the body. Research published in Postgraduate Medicine found that bioidentical progesterone plays a protective role in breast health.
“Bioidentical progesterone has been shown in many studies to decrease breast cell proliferation,” says Prouse, “whereas the synthetic form of the hormone, progestin, has been shown to increase breast cell proliferation.” Prouse has been taking bioidentical progesterone for the past five years. “I have an extensive family history of breast and ovarian cancers and a natural tendency toward estrogen dominance,” says the 47-year-old. “My body is in better balance now than it was in my early 40s.”
Seeing how out of balance my hormones were was a wake-up call. As women, we juggle so many different things, and it’s easy to fall into a stressed and sleep-deprived state and let our diet slip to something that’s far from perfect. For me, I realized that a lot of my late-afternoon fatigue was due to my hormone imbalance, and since taking steps to correct that, I have felt a huge energy boost and am sleeping better and waking less through the night.
I started on a supplement regimen aimed at supporting my adrenal glands, cleaned up my diet and focused on yoga as a means to handle stress. I also started visiting an osteopath regularly. While I was prescribed a bioidentical progesterone cream, I have yet to try it. The other methods seem to be working, and my doctor suggested that I retest my hormones to see how they’ve changed before using my original prescription. While there are no guarantees in cancer prevention, I feel empowered to be taking positive steps toward better health.