Contraceptives 101: Your Guide to the Pill, Condoms, IUDs and More

In 1995, long before romance was complicated by things like Tinder and Facebook, Seinfeld’s Elaine Benes coined the term “sponge-worthy,” to describe whether a man was worth sleeping with, while rationing a small personal stash of her favourite contraceptive sponges after they were taken off the market. A trailblazer for sexually liberated TV characters like Girls’ Hannah Horvath and Sex and the City’s Carrie Bradshaw, Elaine showed prime-time viewers that women had taken reproductive responsibility into their own hands, whether that was by using a sponge, a diaphragm (Carrie’s method of choice) or their popular sister, oral contraceptives.
Twenty years later, in the age of fourth-wave feminism, hook-up culture and Goop-level vigilance over what we put in our bodies, the 55-year-old pill is looking as out of date as Elaine’s frumpy wardrobe. Taking a pill at the same time every day can be a nuisance, it doesn’t protect against STIs and its potential side effects, like mood changes or a lower sex drive, are deal breakers for some. Nearly half of all pregnancies in North America are unplanned and the pill has a failure rate of eight to nine per cent. So some women are making defiant personal choices when it comes to enjoying their sex lives.
For Cathleen*, a 30-year-old publicist in Toronto, that’s using the withdrawal method, the third most commonly used method of contraception in Canada, according to the Journal of Obstetrics and Gynaecology Canada. “I used the pill throughout university but found that taking it on a daily basis at a consistent time was inconvenient,” she says. She and her husband started to “pull out and pray” about four years ago and are comfortable with the 20 per cent chance of pregnancy that comes with withdrawal. Other women in steady relationships are combining withdrawal or condom use with the old-school rhythm method, for which you track your menstrual cycle so you know when you’re ovulating. It’s also gaining a higher digital profile—this fall, Apple’s iOS 9 will allow users to map their periods, and apps like NaturalCycles monitor your cycle when you input your temperature (your basal body temperature rises after ovulation). The app has about 50,000 registered users in 89 countries, including Canada, with an average age of 27. Rumours of the next update of NaturalCycles involve integration with the Apple Watch, removing the need to take your temperature orally every morning. But Dr. Dustin Costescu, assistant professor and family planning specialist at McMaster University, cautions this type of hormone-free birth control should only be used by couples ready to accept the consequences of an unintended pregnancy. “If you get it wrong, you’ve had intercourse on a fertile day, so your risk of pregnancy is actually very high,” he says.
Taking the pill means ingesting artificial hormones, something that many of today’s health-conscious women are choosing to steer clear of. Holistic nutritionist Joy McCarthy says she stopped taking the pill to address underlying hormonal imbalances, adding that her clients often ask about alternatives. “I’ve had dozens of clients go off the pill and not a single one reports back that they wish they hadn’t,” she says. Costescu, who is also a member of the Society of Obstetricians and Gynaecologists of Canada, has seen similar patients at his clinic in Hamilton, Ont. “[They have] concerns about the environmental impact of these hormones on our drinking water and concerns about lifetime exposure to hormones,” he says. “While, by and large, it probably is safe, I’d rather a patient use a method that they’re motivated to use than one that’s causing them these kind of fears.”
The fear factor is very real. In a small proportion of women—those who smoke, have high blood pressure, are over 40, or have other risk factors for heart disease or stroke—oral contraceptives increase the risk of blood clots. A UK study released in May indicated that some forms of the pill containing both estrogen and newer progestins could pose an even greater threat in users. Though this might sound alarming, the risk of developing a blood clot from the pill is lower than the risk of getting one when pregnant or in the weeks after giving birth.
It doesn’t help that teenagers are often afraid their parents will find out they’re sexually active. “I first started on birth control when I was 16 or so, and I knew that I didn’t want to use the pill—it was too inconvenient and too hard to hide from my parents,” says Sadie*, a 19-year-old student from Vancouver, B.C., who uses the NuvaRing. And because there are few male-led options available, some women may feel pressure from their partner to take the pill, a completely hassle-free option for men, who tend to lose sensation with condoms. While a highly anticipated male equivalent of the pill has yet to materialize, one option on the horizon is Vasalgel. Still in the testing phase, this non-hormonal, long-term, reversible contraceptive is a small polymer that blocks sperm when inserted into the vas deferens (the duct that carries sperm to the urethra).
Awareness of the intrauterine device (IUD) is quickly growing because of positive coverage on sites like The Cut, Salon and Jezebel, and through word of mouth, which was how Madison*, a 35-year-old marketing director, first heard about it. “My family doctor didn’t even know much about this option. I had to ask for it,” she says of the Jaydess hormonal IUD (which the company refers to as an intrauterine system or IUS). Alternatively, copper IUDs are hormone-free. “We have women now who aren’t at home, who travel, who are busy and who are sexually active. Is it realistic from a scheduling perspective to take a pill at the same time every day?” asks Dr. Christine Palmay, a Toronto-based physician who attributes the over 99 per cent effectiveness of these methods to removing human error from the equation. Diana*, a 36-year-old teacher, is now on her second hormonal IUD. She says the only minor downside was the insertion, which can be painful. There are fewer issues in women who’ve already had children, which is perhaps why they’re gaining popularity among women in their 30s. “For me, the cramping was gone in a few days and I’ve loved it ever since,” says Diana. “It’s definitely worth it for years of hassle-free birth control.”
Hassle or not, the most common method of birth control in Canada is the male condom, chosen by 54 per cent of all contraception users (the pill comes in second at 43 per cent). Condoms have a pregnancy-prevention rate of 97 per cent when used properly. They’re also one of the only methods that help prevent sexually transmitted infections, a major boon when you’re choosing short-term partners. “My relationship status is ‘inconsistent,’ and condoms are just the easiest and most effective thing to use,” says Liz*, a 32-year-old publicity manager in Toronto. “Why risk it, right?”
We asked women to share their birth control choices in 140 characters or less.
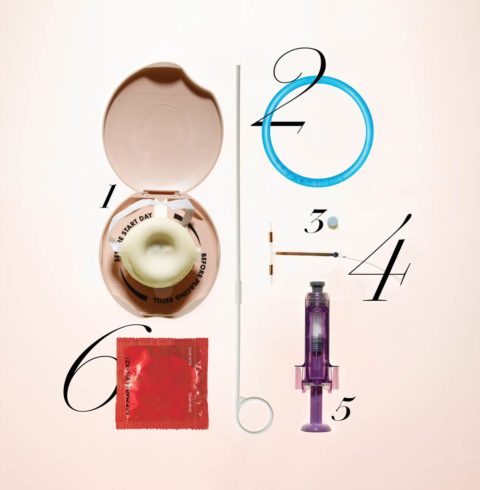
1. DIAPHRAGM
Carrie Bradshaw’s method of choice in Sex and the City
2. NUVARING
“You only have to worry about it once a month. Also, it’s extremely easy to hide.”
—Sadie, 19
3. ORAL CONTRACEPTIVES
“It’s convenient and I like the side effects of an easier period and clearer skin.”
—Laura*, 26
4. MIRENA IUD
“A side effect is you get little to no period, which I love.”
—Diana, 36
5. NEXPLANON IMPLANT (Not available in Canada)
“I get to be responsible but take the daily responsibility out of it.”
—April*, 31
6. CONDOMS
“I feel almost 100 per cent safe when I use them together with the pill.”
—Jessica*, 23
JAYDESS IUS
“Set it and forget it!”
—Madison, 35
PULL OUT METHOD
“I’m financially stable, married and would be happy to have a babe in my life, although hopefully it keeps working for a bit longer!”
—Cathleen, 30
*names have been changed